Good morning! It has been 341 days since the first documented human case of COVID-19. The newsletter comes a little late this morning due to an issue with the scheduler.
Today, I’ve gone in-depth into recent studies on the transmission risks aboard aircraft. I could study this topic for years, though, and not get it 100% right. Also, some headlines and a response about mouthwash in the Talk Back section.
I can’t believe this week is on its way out already. Have a great weekend.
As usual, bolded terms are linked to the running newsletter glossary.
Keep the newsletter growing by sharing it! I love talking about science and explaining important concepts in human health, but I rely on all of you to grow the audience for this:
Now, let’s talk COVID.

Remdesivir FDA-approved to treat COVID-19
Yesterday the FDA formally approved remdesivir for the treatment of severe COVID-19 in hospitalized patients. You can read the press release from Gilead here: https://www.gilead.com/news-and-press/press-room/press-releases/2020/10/us-food-and-drug-administration-approves-gileads-antiviral-veklury-remdesivir-for-treatment-of-covid19
This is based on 3 peer-reviewed clinical trials, which demonstrated some benefit for the use of remdesivir. As I’ve mentioned before, remdesivir is a tool that may help the overall healthcare system deal with the pandemic. It has been convincingly demonstrated to reduce the length of COVID-19-related hospital stays; the faster people get out of the hospital, the less likely they are to get infected with something else while there and the more beds are kept free for other patients to be treated.
This approval supersedes the previous Emergency Use Authorization for remdesivir in the same patient population. In addition to the approval, the FDA created a new remdesivir EUA that applies to use in hospitalized pediatric patients under the age of 12. This is a very small patient population, thankfully.
UNICEF stockpiling syringes in anticipation of a COVID-19 vaccine
UNICEF, a UN organization, is responsible for a number of child-oriented programs around the world. In conjunction with WHO, UNICEF is heavily involved in child vaccination campaigns. Yesterday they announced that they will be stockpiling 500 million syringes to help with an anticipated COVID-19 vaccination campaign, something that will help to prepare infrastructure for the distribution of whatever vaccine is ultimately deployed.
Read the press release here: https://www.unicef.org/press-releases/unicef-stockpile-over-half-billion-syringes-year-end-part-efforts-prepare-eventual

What am I doing to cope with the pandemic? This:
Writing this newsletter
Yesterday was a busy day, and that in-depth piece you’re about to read took a lot of work. But it actually does help me live through this pandemic to write to all of you each day.

Air travel safety
I’ve seen a lot of news recently about recent studies looking at the odds of infection during passenger air travel. The study that made the biggest splash was sponsored by the US Department of Defense, looking at transmission dynamics inside 767 and 777 Boeing aircraft.
This study found that under test conditions it appeared that the risk of transmission inside an aircraft is very low, but I’d like to walk through what they did and how what they did may have certain important limitations. Thankfully, because this is a US government research report and I am a US taxpayer, I don’t have to worry about copyright to just quote it directly.
The experimental setup in this study used simulated virus particles. Specifically:
The test process involves the use of tracer aerosols and two types were used in the commercial airframe tests: 1 µm fluorescent microspheres and 3 µm DNA-tagged microspheres. Discrete fluorescent particle counters were used for real-time aerosol sampling and selective detection of the fluorescent tracer particles. For the effort, 42 IBAC sensors were loaned from the DHS Science & Technology Directorate and the National Guard Bureau Weapons of Mass Destruction Civil Support Teams, in coordination with MIT-Lincoln Laboratory and L2 Defense respectively.
Translating from the awful conglomeration of jargon that happens when scientific literature and government reports collide, essentially what we have here is a system where simulated aerosolized particles were created. These particles were created in two sizes, depending on their type. Fluorescent (glowing) particles were made at a diameter of 1 micron (that’s 1 millionth of a meter) and DNA-tagged particles were made at a diameter of 3 microns. The choice of fluorescence and DNA tagging was to make it possible to detect these particles easily; DNA-tagging just means that a molecule of DNA was attached to these particles that allowed them to bind to other DNA and thus be detected by normal techniques for DNA sensing.
These convoluted detection techniques were used because these particles are very small. It is hard to see small things, it turns out. This may sound silly, but in reality the inability to see small things is the biggest problem that we face in the study of modern biology. Much of biology in the 20th and 21st centuries has been about finding new ways to see very small things, even indirectly. A great way to win a Nobel Prize in one of the areas that covers biology is to find a new method of visualizing some biological process.
The sizes of the particles was a deliberate choice; these sizes are both smaller than 5 microns. This size is much larger than a single SARS-CoV-2 virus particle, let’s keep in mind. However, it is in the range of sizes for aerosolized respiratory particles, which can contain infectious numbers of SARS-CoV-2 particles. It’s more important to simulate these small respiratory aerosols—made of fluids that we expel—than individual virus particles.
The authors of the study specifically selected particle sizes based on previous work looking at the population of SARS-CoV-2 particles in specific droplet sizes:
SARS-CoV-2 viral shedding numbers in literature vary, with no definitive answer on the number or size of particles an infected patient releases. Liu et. al (2020) determined that for SARS-CoV-2 aerosol collections in a clinical setting, viral RNA concentrations are maximum in a distinct bimodal distribution with one peak between 0.5 and 1 µm, and the other above 2.5 µm, leading to the tracer sizes utilized here (1 and 3 µm).
As described here, 1 micron and 3 microns are within the range of 2 separate peak particle sizes for virion count from a previous study. They wanted to cover 2 approximate aerosol sizes that were expected to deliver a lot of virus. This makes sense to me!
However, this is where we run into our first methodological issue. We don’t actually have a good study of transmission dynamics of SARS-CoV-2 right now. Most of our information on transmission comes from the large global study that we are all participating in whether we like it or not. Our findings from this are observational and not conducted by a rigorous design. The reality is that we just don’t know what particle sizes are likely to transmit the virus in various conditions. It’s possible that different particle sizes are generated inside an aircraft than were generated in the study that informed these particle sizes.
That’s the first issue. Still, we have to do the best that we can do design experiments of this nature.
Let’s move on to the rest of the design. The authors also created a mechanism for dispersing these particles in an aircraft, using a mannequin. It looks pretty creepy.
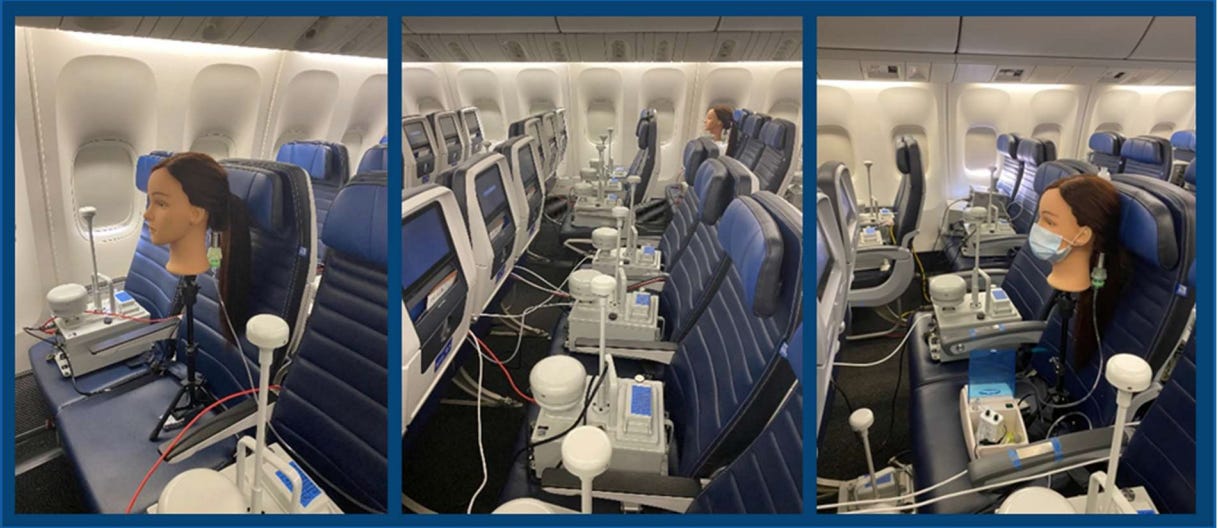
Image is three pictures of the interior of an aircraft. In the leftmost picture, the head of a mannequin, attached to aerosolization apparatus, is in the middle seat of a 3-seat windowed row. In other seats, detection apparatus have been placed to count particles that are delivered by the aerosolization apparatus. In the middle photo, we see the center row of the aircraft with detection machines seated in the center, 4-seat row as well. The mannequin is visible in the background, far from the seats that are in the foreground. This establishes that aerosols that traveled some distance could have been detected. Finally, the leftmost image shows the mannequin seated again, but with a mask over its mouth to simulate this condition.This is an interesting setup. In principle, we have all of the things that we need to see aerosol transmission of virus in an airplane. We see that unmasked and masked conditions can be tested. There are detectors are considerable distances. An actual airplane with an actual airplane air movement system is being used. However, here I also have some methodological concerns.
People in aircraft are not floating heads. They do not sit for hours with their heads facing perfectly forward, emitting constant bursts of aerosolized particles directly forward over time. People flying in planes talk, they get up, they move around. They adjust their masks inappropriately, moving them to do horrible things like drinking water or eating cookies. On a plane there is no perfectly masked condition or perfectly unmasked condition.
Let’s be very blunt, though: I’m not advocating that we need a perfect model to do this experiment. The perfect model would be unethical, using actual people in masked and unmasked conditions, with controlled releases of COVID-19. At that point I’m not sure we could even call it a model anymore—we would just be studying transmission of virus. I don’t think that would be appropriate to do.
We do have to work with what we have, so I want to be clear there is a purpose to my pointing out these limitations: they help to inform the conclusions that we can draw from the results of the work.
And the results were rather interesting. Here is a figure from the study, looking at dispersion of particles from seat 47B and 47E in a 777 aircraft, under various masking vs unmasking conditions, simulating breathing and coughing:

Image is a complicated data figure, showing a color-coded distribution of how many particles were detected when released from a specific seat in the aft section of a 777-200 Boeing aircraft fitted for passenger travel. The color code shows us three color codes; red, for seats that received more than 1% of emitted particle concentration, yellow, for seats that received between 0.01% and 1% of emitted particle concentration, and red, for seats that received more than 1% of emitted particle concentration. The color code is not meant to indicate which zones are safe and which are not; they are just meant to indicate the order of magnitude of exposure.We can see in this example figure that exposure is relatively low from simulated breathing with a mask on, but what I can’t tell you is whether this low level of exposure would have been infectious under real-life conditions. I’m also a little troubled by the fact that we are looking at an assumption here of only one infected patient on the aircraft. I think that’s a limitation, too. What is the exposure if you have two infected patients? Three? 10?
At present, the population of people who have ever been infected with SARS-CoV-2 in the US is larger than the population of the country’s largest city. A notable population of people are currently infected with the virus as well. In a plane that holds hundreds of people, can we be certain that the maximum infected population would only be one person?
I imagine that there would be additional risks posed by multiple positive individuals on board an aircraft.
I cannot book-report the full results of the study here. It is in-depth and substantial. But I can summarize my reactions to its conclusions:
Given the data captured during this most recent round of testing, and coupled with existing literature and a growing consensus on COVID-19 risks, the following recommendations regarding troop transport on commercial airlines can be conveyed.
For the 777 and 767, at 100% seating capacity transmission model calculations with a 4,000 viruses/hour shedding rate and 1,000 virus infectious dose show a minimum 54 flight hours required to produce inflight infection from aerosol transmission.
This conclusion may be true for the assumptions stated, but let’s be totally clear: there are a bunch of assumptions being made here. We do not know the minimum infectious dose; there are viruses in which the minimum infectious dose is 10 particles. The range in the literature for SARS-CoV-2 reports between 300 particles and thousands of particles required for infection, but since we do not have robust studies of asymptomatic infection there may be a substantial number of infections that occur after much smaller exposures. I do not think a 1,000-particle minimum dose is a reasonable estimate. This is clearly a study that was conducted by people with more experience in engineering and indoor environments than in virology, who thought this was a good enough model. I do not think this is good enough.
Additionally, we do not know how having live people in the aircraft would impact the results. We do not know how having an “experienced” airplane, with potential issues in air system maintenance, a questionably-cleaned interior, and other potential problems might change the results.
Aerosol exposure risk is minimal even during long duration flights, but typically highest in the row of an index patient. Rows in front and behind the index patient have the next highest risk on average.
The only part of this conclusion that I can support is that exposure would be highest in the row of the index patient, as well as in rows immediately behind and in front of that patient. If you fly, try not to sit near someone infected with COVID-19. Not a very good recommendation, I know. It’s not like they wear a sign saying they’re infected.
While there is a measurable difference in middle vs aisle or window seat, there is no practical difference at these high overall reduction levels.
I don’t know what this means; we’re comparing levels between seats when we don’t actually know what an infectious dose actually is. I can’t make much of this conclusion.
As testing did not incorporate large droplet contamination, recommend continued disinfectant cleaning and mask-wearing, or testing this transmission mechanism in an alternative methodology.
Here the authors note a significant limitation of the study; they did not look at large droplet transmission, which is still thought to be a substantial mechanism of transmission. While it might be limited by a mask, we do not know if a mask is perfect protection for the person sitting next to you.
The benefit of commercial airframes, and the validity of these recommendations relies on the combination of a HEPA-filtration recirculation system and the high air-exchange rate, which is not matched by other indoor venues, including most hospital and biosafety-level 3 laboratories.
This isn’t really about the study; it’s about the fact that aircraft have good air-filtering systems. While this is true, I don’t think that the study investigated what happens if you intentionally compromise the air filtration system on an aircraft. What if the HEPA filter hasn’t been replaced recently? What if it is punctured unknowingly? This wasn’t examined.
Overhead gasper supply (on or off) does not make a significant impact on aerosol risk and could continue to be used primarily for traveler comfort.
“Gasper” is the name of the little gadget above an airplane seat that lets you blast yourself with air. They looked at conditions where the gasper was on or off and compared them. The data do support the idea that the gasper doesn’t have any effect, and I think this is a good conclusion.
Contact tracing should be limited, and is unlikely to be necessary for aerosol transmission, but may be necessary for large droplet transmission in the seats immediately neighboring an infectious passenger, or from uncertainty in human behavior (i.e., talking to a neighboring passenger while eating or drinking without a mask, which is not tested here).
This is not supported by the data. We simply do not know what the minimum infectious dose is. If there is one passenger who tests positive on an airplane, asymptomatic infections may have occurred in nearby passengers one or two rows ahead of them. The authors note here how idealized their conditions are—”uncertainty in human behavior.” The example they provide describes typical human behavior on an aircraft. Given that this type of condition is not represented here, I don’t think that the experiment adequately models the aircraft experience to tell us what is safe. Still, I don’t think that makes this work useless—and I’ll explain why later on.
Flight deck exposure risk is extremely unlikely, as the ECS system supplies separate air to this portion of the aircraft.
This sounds reasonable. However, they didn’t do any experiments to support it. They’re just making an assumption here. That said, unless you are the pilot of a commercial airliner or you fly on a commercial airliner where the pilot is infected with SARS-CoV-2, I don’t think this really matters. It’s more likely that a passenger is infected than that the pilot is infected, so I wouldn’t be too worried about this.
Additionally, during boarding and deboarding, the following recommendations should be considered:
Keeping air supply and recirculation mode (HEPA-Filtration) operating is critical. Ground supply and APU behave similarly, but there is likely more uncertainty with variations in ground supply flow rates and suppliers, since the test team was only able to test the single provided system.
I agree with this. I do think the results indicate that the air system on an aircraft does a significant job in reducing particle counts in the air. Convincing information is presented to show that you are exposed to fewer particles inside an aircraft than you would be inside a typical home. However, it is not at all clear that this makes a meaningful difference in your ability to become infected.
However, since there are always going to be people who need to fly for truly essential reasons, we should at least try to give them their best chance for success. To do that, we need to keep aircraft air systems in their best maintenance condition possible.
Jetway exposure risk from an infected person already sitting in the airframe was low with reductions for the 777 and 767 terminal of 99.999%.
I would agree with this conclusion, that the risk to someone in the jetway is low from someone seated in the aircraft. They did look at jetway exposure and they did show vanishingly low amounts of particles detected.
Loading passengers in smaller groups and allowing distance on the jetway is likely beneficial to maintaining social distancing guidelines, but simulated infected personnel within these jetways was not tested.
I also think this is a good recommendation. It is clear that there is a maximum distance that virus particles can travel inside an aircraft. By boarding in small groups, we minimize the chances of intermixing between passengers and hopefully keep exposures restricted to just those who boarded and sat with any infected passenger(s).
Now, as you can see, I don’t think most of the conclusions of this study are well-supported by the data and I believe the study is compromised by methodological flaws. However, I do not think this makes it a useless body of work. I would make the following conclusions from my evaluation of the data:
I am convinced that masks on an aircraft meaningfully reduce dispersion of aerosolized particles. Everyone should wear a mask when flying, and I think this study convincingly demonstrates that.
I am also convinced that an aircraft air system is helpful in reducing aerosolized particles. This probably means that by comparison to an equal amount of time spent in another indoor environment with an infected person, you are less likely to become infected when inside an aircraft with an infected person. However, this is dependent upon how close you are to the infected person, because distance still matters. I do not see anything here to convince me that social distancing aboard airplanes may be dispensed with, as some airlines have decided to conclude.
These are limited conclusions but I think they are meaningful for anyone who must travel. Wear a mask and insist that everyone else must wear a mask. Don’t panic about the fact that you have to fly; the air system will be helpful for you.
I would still avoid flying, however, unless absolutely necessary. There have absolutely been documented cases of COVID-19 transmission on airplanes. Most of these cases, however, occurred in the time before mask mandates on aircraft were instituted, something which I do find reassuring.
Another point to note is that the 6-foot distance that we have all been advised to social distance with is partly based on data from an aircraft. Specifically, a study was published in The New England Journal of Medicine about dispersion of SARS-CoV-1 in aircraft: https://www.nejm.org/doi/full/10.1056/nejmoa031349. This study suggested that a distance of 6 feet might be sufficient to avoid exposure to SARS-CoV-1, the relative of SARS-CoV-2. That strain of SARS-CoV happens to be a lot less contagious than SARS-CoV-2, but that’s beside the point. Our rule for social distancing is based on air movement on an airplane and a documented situation of virus transmission under aircraft conditions.
In that study, three aircraft were examined. Two were Boeing 777-300 planes, and one was a 737, but the events studied occurred more than a decade and a half ago. In the meantime there have been some changes to the air systems installed on planes, but when you book a ticket you can’t guarantee that you’re getting a newer plane or an older one. There are plenty of airframes in service that are 15 years old.
I think what all my opinions here sum up to is this: if you do not have to fly, don’t fly. If you have to fly, then you have to fly. The risk of COVID-19 shouldn’t stop essential travel by otherwise healthy individuals, but everyone has to make their own conclusions about what essential means. There is no perfectly protected situation. There are risks associated with air travel, both COVID-related and otherwise. By traveling on an aircraft, you are taking a risk that you can try to mitigate by choosing an airline that has good policies and adhering to those policies yourself.

The last issue received the following comment, about the mouthwash study piece that I headlined, from reader George Stanchev:
Regarding the mouthwash, I agree that once the virus invades the LRT, it is useless. However many times COViD starts as URTI and it is localized to the nasopharyngeal mucosal epithelia. During this time, gargling could reduce viral load in the mouth thus reducing transmission risk and symptoms. Please check ELVIS trial out of university of Edinburgh. Same team is running similar trial for COVID. While I agree it won’t cure it, it might offer benefits when applied early in the infection cycle.
I provided the following reply:
Thanks for pointing out that this has been studied elsewhere--I think this is worth noting, but I do think we should be clear on what's data and what's speculation.
I will concede the point that it is worth studying; there are certain limited conditions under which I could hypothesize--only hypothesize, mind--that use of mouthwash could help to limit an infection or otherwise make it abortive.
For example, mouthwash use within an hour of exposure might sanitize the mouth sufficiently to reduce the input dose before all potential local infection events have occurred. In this way, it might be mildly prophylactic. To my knowledge, this hasn't been demonstrated anywhere. The study that I was sharing didn't demonstrate this because it was not a clinical study.
I am familiar with the ELVIS study; it was a test of the effect of gargling on the transmission and duration of colds. I do not think that it is relatable to mouthwash. Hypertonic saline (aka really salty gargling water) is not the same thing as Listerine. There are a number of mechanisms that might explain why hypertonic saline gargling could affect disease course and transmission in the common cold, which is a purely upper respiratory illness. The common cold is not COVID-19, though, so I just don't think that these results are portable. We will have to see the results in ELVIS COVID-19 before making conclusions, and right now I do not think we have any data on this.
That said, mouthwash is not an antiviral drug. We have not seen it studied as one, and we cannot conclude from the currently available data that it will have any effect on COVID-19. By the time a person is infected, their cells are producing new virions at high rate. Mouthwash may help to destroy viruses present in the mouth, but it won't affect those in the nasopharyngeal space in its entirety, nor in the lungs. It will also not prevent the formation of new virions. It is possible that it could reduce the kinetics of spread through the body in an early infection, but again, we need an experiment to study this and we don't have one.
At the end of the day, hypotheses are cool. Speculation is interesting. Neither should inform behavior. The best way to deal with COVID-19 is to avoid getting it. If that fails, the next best way to deal with it is to seek the advice of a physician. But if you want to use mouthwash a couple times a day, I don't see how it could hurt if used as directed. It's generally safe for human use, or it wouldn't be on the market as mouthwash. Just don't drink it, inject it, or use it any other nonstandard way.
Join the conversation, and what you say will impact what I talk about in the next issue.
Also, let me know any other thoughts you might have about the newsletter. I’d like to make sure you’re getting what you want out of this.

This newsletter will contain mistakes. When you find them, tell me about them so that I can fix them. I would rather this newsletter be correct than protect my ego.
Though I can’t correct the emailed version after it has been sent, I do update the online post of the newsletter every time a mistake is brought to my attention.
No corrections since last issue.
Thanks for reading, everyone! Have a great weekend!
See you all next time.
Always,
JS



